

The 2020 No Surprises Act (NSA) established new federal protections against surprise medical bills and balance billing, most of which took effect January 1, 2022. Below is a summary of the major No Surprises Act requirements and what they mean for you.
To learn more about ACEP’s many years of advocacy on this issue that led up to this law, click here.
The No Surprises Act:
The No Surprises Act does NOT make any changes to your EMTALA obligations, including the medical screening exam and stabilization definitions and requirements that have been in place for decades.
However, the law DOES extend the ban on balance billing to additional services that patients may receive in conjunction with an emergency visit even after they are stabilized—a new concept known as “post-stabilization services” in the law.
Thus, a patient coming to your ED to be treated for a medical emergency cannot be balance billed for any of the out-of-network services they receive up to the point of stabilization, NOR for the care they receive once they are:
The balance billing protections end when you discharge the patient. They also can end when under your clinical judgment the out-of-network patient could have been transferred to a participating facility safely and without undo financial burden using a non-emergency form of transportation (like the patient’s car, a bus, or a taxi), AND the patient signs a notice-and-consent given to them by the subsequent clinician.
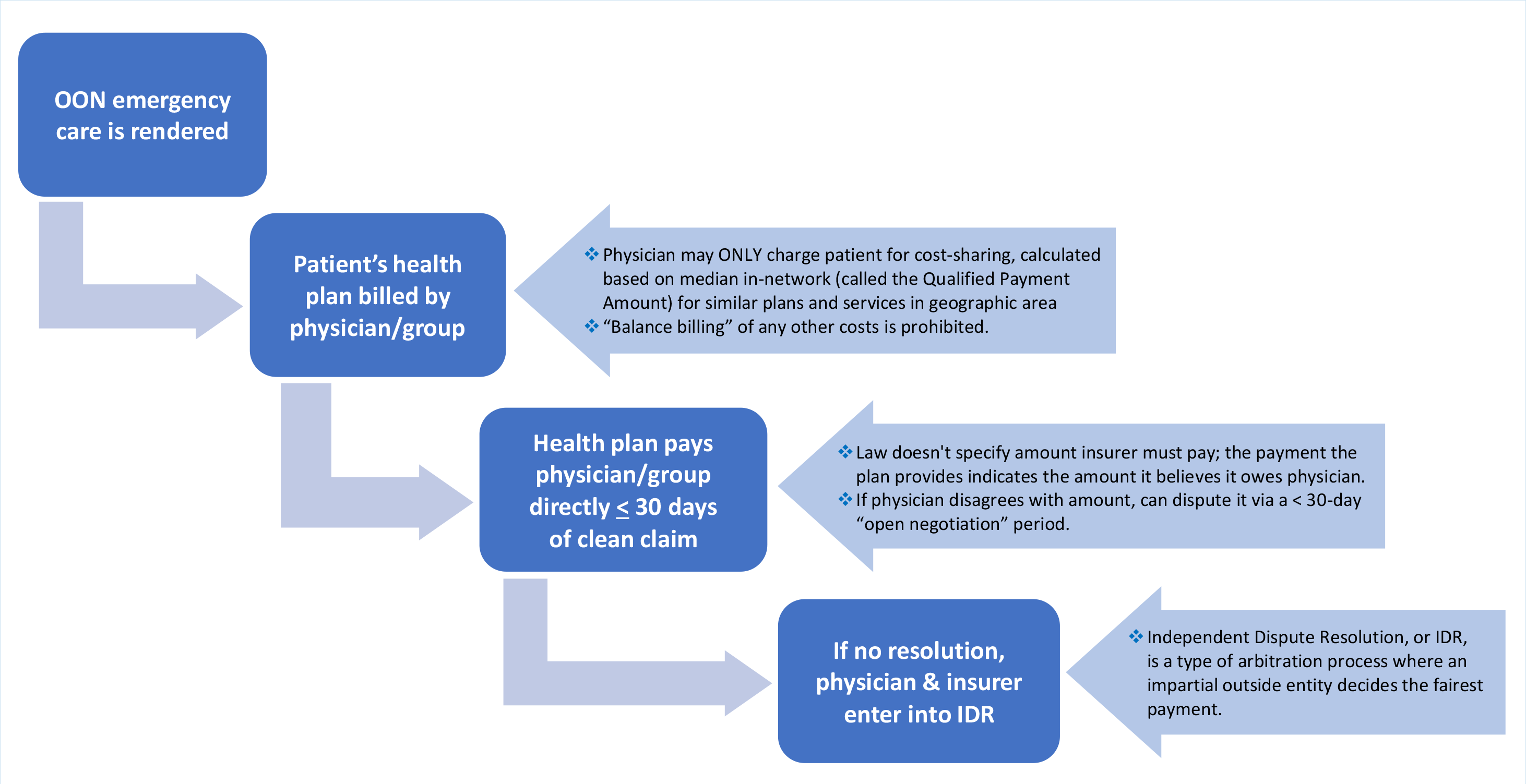
The online IDR portal opened April 15, 2022. Generally, the IDR process will follow a “baseball-style” approach, following these steps.

ER physician submits claim to patient's insurer. The patient is only responsible for any costs as if in-network, and is now out of the middle.
Physician/group can dispute the amount during the 30-day open negotiation period.
If that fails, either party can take the dispute to IDR using an online portal. They'll select an arbiter from a pre-vetted list of IDR entities. Both parties must pay the IDR fee up-front ($200-500 for one claim; $268-670 for "batched" claims of similar services with that same insurer).
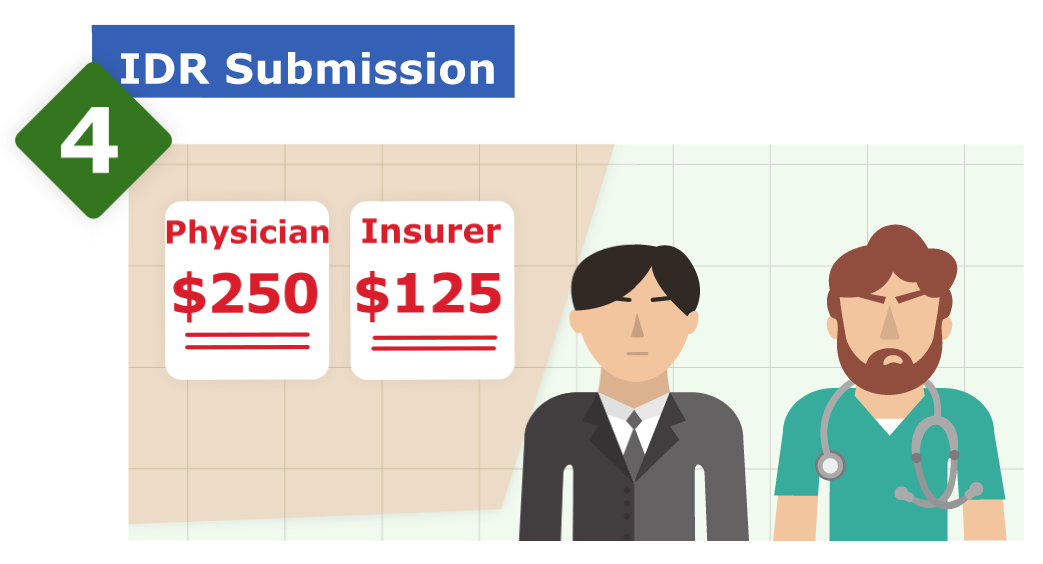

An impartial reviewer evaluates both submission and chooses one of the two payment amounts within 30 business days after the reviewer is selected. They can't come up with their own amount; it must be one of the two proposed.
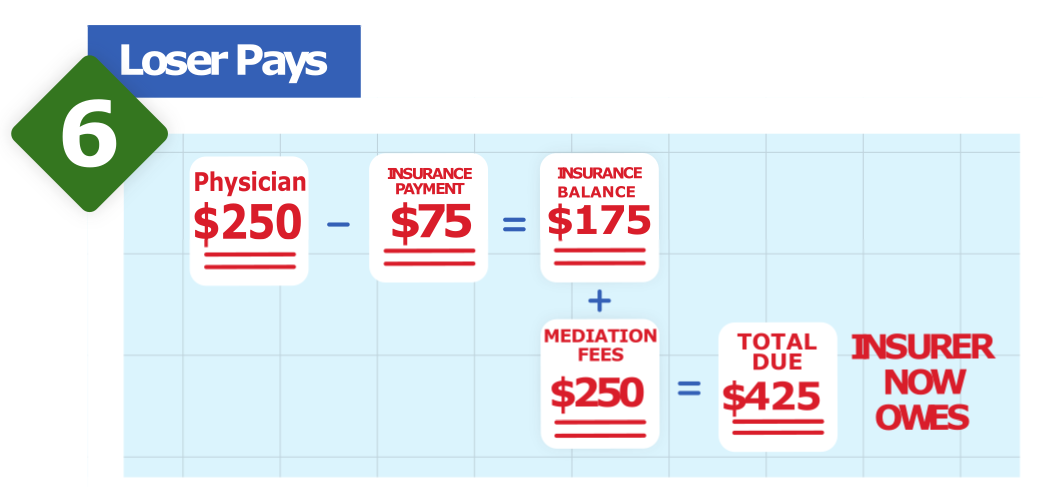
The loser has to make the other side whole and pay for the IDR fee within 30 calendar days. The winner gets their filing fee refunded within 30 business days.
Remember, this federal IDR process will only be used for disputes for which no specified state law applies (see section below).
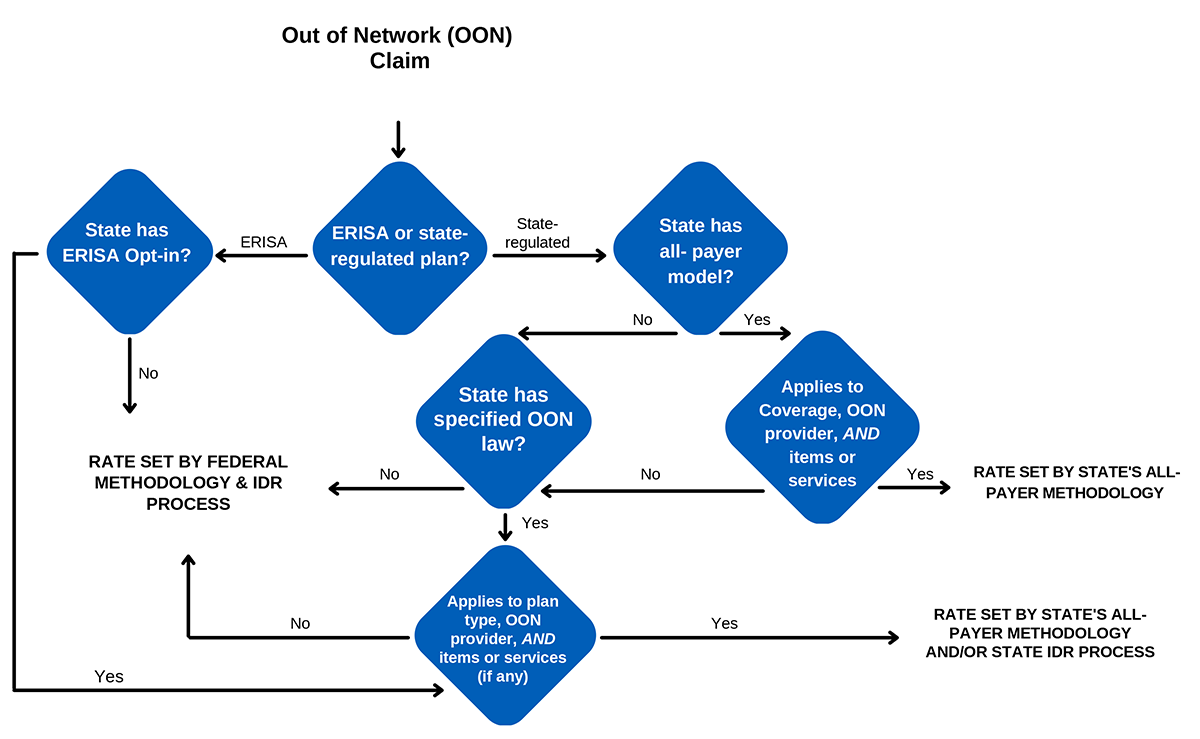
1) For emergency patients under a state-regulated insurance plan (such as employer-sponsored commercial plans):
2) For federally regulated insurance plans (such as ERISA/employer self-funded or federal Marketplace plans under the ACA), the federal law’s initial payment and IDR process governs the OON payment amount. Note: In some states, ERISA plans are allowed to opt-in to the state law.
The federal government has already released guidance designating some states as having a qualifying law. See table below, which will be updated as more guidance comes in on the remaining states.
State/Territory
Direct Enforcement of NSA
Adverse Determinations
IDR Process
Patient-Provider Dispute Resolution
Federal Government (CMS)
Federal External Review Process
Federal IDR Process applies
Federal process applies
Federal External Review Process
3 Alaska Admin. Code § 26.110(a) is a specified state law that will apply for purposes of determining the out-of-network rate with respect to items and supplies furnished to individuals in an insured group health plan, or group or individual health insurance coverage in Alaska by nonparticipating providers, nonparticipating emergency facilities or nonparticipating providers of air ambulance services. Federal IDR process will only apply for services not applicable to the state law.
Federal process applies
Federal Government (CMS)
Federal External Review Process
Federal IDR Process applies
Federal process applies
Arizona will enforce certain provision of the law and the Federal Government will enforce others
Federal External Review Process
Federal IDR Process applies
Federal process applies